The wound healing process involves many complex factors. These may be classified as local factors, systemic factors and organ and species variadility in response to injury. Topical medications should provide a specific desired effect during the appropriate stage healing
8. In this study, we adopted an experimental design including macroscopical and histological evaluations of the wound healing process. Propolis is a natural drug that has been employed extensively since ancient times
1,5,10,11. Khayyal et al.
5, reported that aqueous propolis extract possesses significant anti-inflammatory properties and has successfully reduced oedema in both acute and chronic models of inflammation.
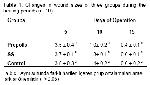
The propolis skin cream appears to have a beneficial effects on healing burn wounds 10,12,13. It was also reported that propolis has a therapeutic effect on wound healing, inflammations of the skin and other skin lesions 1,4. In this study, all wound sites was healed in17 days after surgery. The wound contraction and wound healing rates of propolis were higher than other groups.
According to the results of the present study, including macroscopical, qualitative, and microscopical analyses propolis has a higher healing performance than other groups.