Subject and Settings
The patient, a Caucasian female born at 366/7 weeks of gestation (2.215 g, 45 cm) via ceserean section after the first pregnancy of a 28 year- old mother, was diagnosed with PWS at 15 months of age.
The study included a 3 6/12 –year-old female subject with a height of 92 cm and a weight of 13,5 kg. Amniosynthesis was done with the suspicion of Down syndrome in 6th week of the gestation. In addition, the rate of increase in abdominal circumference was found to be below normal range. During the first 2 months after birth, above-normal sleeping hours and weak head control had raised an attention. At 6 months, her parents was referred to a pediatric neurology clinic with complaints of abnormally low level of reactions and activity. Pre-diagnostic was thought to be PWS which was later confirmed by FISH test. At 8 months the subject was referred to Hacettepe University Faculty of Health Sciences Department of Physiotherapy and Rehabilitation because of hypotonia. Both parents are graduates of high-level education program and were thoroughly informed about PWS at the beginning.
Observational parameters related to physiotherapy and rehabilitation consisted of investigation of social, emotional, cognitive, motor and sensorial characteristics. Furthermore, developmental reflexes was noted and for detailed analysis of motor development Gross Motor Functional Measurement (GMFM) was used14. GMFM is a standardized observational test designed to evaluate the changes over time in motor development in children with developmental disabilities like cerebral palsy and Down syndrome. It consists of 88 items and 5 subscales (supine-prone, crawling, sitting, kneeling, standing-walking and running) parallel to normal developmental milestones.
Parental informed consent was obtained after detailed information was provided about the ongoing case study.
Baseline Assessment
Initial Evaluation at 8 months
The subject was fed with the help of a baby bottle because of weak sucking. Starting at 5 months, liquid foods (ie. yoghurt, fruit juices) were included in feeding. Frequent fevers were present.
Body Composition: At 7 months body weight was measured as 7.5 kg and head circumference was 42.5 cm (evaluated as normal).
Motor Development: Severe hypotonia was present. Motor activities including head control were absent. “Floppy infant” appearance was present. GMFM score for the first evaluation was “0”.
Cognitive Status: No reactions were present in response to audible and visual stimuli and the subject was not interested in toys or objects. No recognition of father, mother or any other person.
Social Development: No social behaviors were present.
Emotional Development: High-pitched crying was present. No sign of smiling or any other facial expressions.
Sensorial Status: Visual and auditory systems were intact with marked internal strabismus. However, subject was unable to produce meaningful sounds.
Physical Appearance: Compared to body size, feet and hands were small in appearance. Almond shaped eyes and well-rounded cheeks were marked features of the subject.
Reflex Development: Asymmetrical tonic neck reflex, amphibian reaction, symmetric tonic neck reflex, corrective and protective reflexes were absent.
Neurodevelopmental Treatment Approaches
Following initial evaluation, a physiotherapy and rehabilitation program based on Bobath Neurodevelopmental Treatment Approach was initiated for 2 days/week15. The program consisted of tonus regulation, positioning, facilitation of head control, balance and protective reactions, sensory-motor and cognitive training, and techniques aiming to enhance postural stability and proprioception. In parallel to the increase in age, activities focusing on muscle strengthening and aerobic endurance were included in the rehabilitation program.
Parental training was provided to ensure that home based therapy was sufficient enough.
Observational Findings
Neurological Development: At 10 months activities of independent sitting and passing objects from one hand to another were gained. At 12 months some spelling and mimicking speech voices were obtained. At 12 months the subject was observed normal in the aspects of fine motor and speech skills, however gross motor evaluation was concordant with 9 months of normal development.
At 18 months, standing with the help of a holding, spelling of unmeaningful words (dada) and demonstration of body parts were observed. At 24 months the subject's status in fine motor activities and speech was in concordance with 12-15 months of normal development, whereas gross motor development matched with 11-12 months of normal development. At 24 months there found to be an increase in the number of words used by the subject. Head circumference was 45cm at 12 months and 46 cm at 24 months.
Endocrinologic Development
Pediatric endocrine visits were initiated at 23 months of age in parallel with development of oral motor functions and solid feeding. It was noted that her weight was at 50th percentile in between 6 to 12 months and decreased to below 25th percentile after 12 months. Her height had been increasing around 25th percentile until 18th month, however demonstrated a decline to 10th percentile after that age (Figure 1). Laboratory tests revealed subclinical hypothyroidism as evidenced by her normal T4 and FT4 with slightly elevated TSH. All other biochemical tests were in normal range including serum IGF-I. Therefore, her decreased growth rate was explained by subclinical hypothyroidism and Levothyroxine replacement treatment was initiated. Nutritional recommendations were provided for the parents on adequate and balanced feeding.
Findings of 3 years of follow-up
Neurological: At the age of 3 independent walking and speaking up to 5-6 words were accomplished. Hypotonia was persistent throughout the period.
Head circumference was measured as 48cm at 36 months.
Physiotherapy and Rehabilitation
Neck correction reflex, amphibian reaction and sitting balance were evaluated as normal, however, kneeling, standing and walking balance were insufficient.
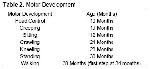
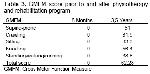
The change in observational parameters after 3 years of physiotherapy and rehabilitation are provided in Table 1. Table 2 presents the overall change in motor development and in Table 3 the change in GMFM is provided.
Endocrinological
Anthropometric measurements for the first 3 years are provided in Table 4. As it is shown in the Figure 1, growth of the subject was observed to be in between 10-20th percentile after initiating thyroid hormone replacement treatment. The subject was followed at intervals of 3 months to keep her TSH in 1/4 lower limits of normal range and with nutritional recommendations.
The subject`s body mass index did not increase over 85th percentile so far and dyslipidemia, cholestasis, gastro-oesophageal reflux, non-alcholic liver diseases and hypertension often seen in PWS patients were not observed in our subject.
The subject was consulted both by a paediatric neurologist and a paediatric endocrinologist. In addition, the level of education of her parents who often followed the current developments in the related literature and collaborate accordingly with the interdisciplinary team, further facilitated the rehabilitation process.