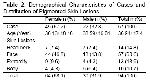
Dermoscopy is a non-invasive technique used in the diagnosis of pigmented lesions and producing more accurate results compared to other methods
2-4,7. Clinical data may not always be adequate in the evaluation of pigmented skin lesions. Dermoscopy is used as a technique to help the physician in the diagnosis of melanocytic lesions like benign melanocytic lesions, dysplastic nevus, and malignant melanoma, in the benign-malignant differentiation, as well as the differential diagnosis of other pigmented nonmelanocytic lesions. It is particularly useful in the correct evaluation of morphological structures which cannot be decided on with naked eye and uncertain pigmented skin lesions, as well as in the pre-operative diagnosis of pigmented skin lesions planned for excision
3,4,6,20-22.
Dermatoscopic diagnoses are given in line with diagnostic algorithms, which are the ABCD rule developed by Nachbar et al.14, Menzies et al.15 method, the seven point checklist designed by Argenziano et al.16, and the pattern analysis developed by Pehamberger et al.13. Dermoscopy uses a two-step algorithm, where the first step involves melanocytic-nonmelanocytic differentiation of the pigmented lesion and the second step consists of the benign-malignant differentiation of the lesion by dermatoscopic criteria24,25. Use of these dermatoscopic methods by experienced physicians increases diagnostic accuracy by 5% to 30%, sensitivity of clinical examination by 19% and specificity 6.2%; thereby the number of patients sent to biopsy decreases by 42%24-27.
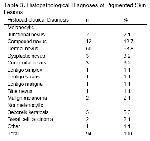
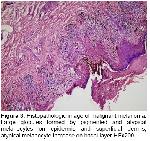
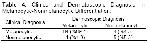
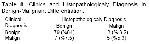
Recently, dermoscopy has become a practical and suggestive method in the differentiation between melanocytic and nonmelanocytic pigmented skin lesions18. Of the nonmelanocytic skin lesions, pigmented basal cell carcinoma in particular can be clinically confused with benign pigmented lesions. Specific dermatoscopic images of pigmented basal cell carcinoma can enable differentiation of any of its types from other tumors28. In a two-year study Demirtaşoğlu et al.29 found that dermoscopy raised the rate of accuracy from 60% to 90% in the diagnosis of pigmented basal cell carcinoma and reported that dermoscopy is a valuable diagnostic tool in the diagnosis of pigmented basal cell carcinoma. White et al.30 who reported a case of pigmented basal cell carcinoma that developed from a burn scar noted that basal cell carcinoma could be clinically confused with malignant melanoma, particularly in patients with dark skin, and stated that dermatoscopic examination helped diagnosis. In our study, dermatoscopic findings of two cases who were clinically considered to be melanocytic were consistent with seborrheic keratosis, and their seborrheic keratosis pre-diagnoses were confirmed with histopathology. A case who was clinically suspected malignant melanoma was found by dermatoscopic examination to be consistent with pigmented basal cell carcinoma, which diagnosis was confirmed by histopathologic investigation. On the contrary, in a case who was clinically given the pre-diagnosis of seborrheic keratosis dermatoscopic findings suggested a melanocytic lesion and the histopathologic diagnosis showed dermal nevus. We established that in differentiating between melanocytic and nonmelanocytic pigmented skin lesions, clinical examination was statistically 96.6% sensitive and 61.5% specific, while dermoscopy was 97.7% sensitive and 88.8% specific.
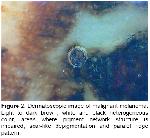
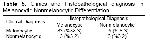
Dermoscopy assumes importance in differentiating between benign and malignant pigmented skin lesions of uncertainty31. Since tumor thickness is the major prognostic factor in melanoma, early diagnosis of melanoma is very important and extremely valuable in reducing the mortality associated with melanoma. In this context dermoscopy assists the physician to recognize malignant melanoma at its onset8,10-17. Blum et al.32 reported that physicians could accurately diagnose cutaneous melanoma clinically at a rate of 65% to 80% and dermoscopy increased sensitivity by 10% to 27% in accurate diagnosis, while Westerhoff et al.33 noted a 39% increase in the latter. Wollina et al.34 emphasized that early diagnosis was the main step in the improvement of prognosis in malignant melanoma, and reported that, having a high sensitivity and specificity in the diagnosis of early melanoma, dermoscopy was an easy-to-use method that dermatologists can employ in the accurate diagnosis of pigmented skin lesions. In a study carried out on 206 skin lesions, Bono et al.35 found that clinical examination was 43% sensitive and 91% specific, whereas dermoscopy was 83% sensitive and 69% specific in the diagnosis of cutaneous melanoma, and reported that dermoscopy was evidently useful in diagnosing very small cutaneous melanoma. Barzegari et al.21 pointed out that computerized dermatoscopic analysis was 93% sensitive and 95% specific in melanoma diagnosis. In our study, of the 2 lesions to which we gave malignant melanoma pre-diagnoses clinically, one was an ulcerated plaque in the palmar area of the hand and the other was a heterogeneous black-gray macula, 2-3 cm in diameter, located between toes. Dermatoscopic findings of both lesions supported our pre-diagnoses, which were then histopathologically confirmed to be malignant melanoma. Clinical and dermatoscopic pre-diagnoses of the lesions were not difficult to give. In our study, lentigo maligna, dysplastic nevus, malignant melanoma and pigmented basal cell carcinoma were accepted as malignant, and it was found that clinical examination was statistically 72.7% specific and 92.4% sensitive, whereas dermoscopy was 80% specific and 97.7% sensitive in the benign-malignant differentiation.
Unwarranted excisions performed on low-risk pigmented lesions located on the face, genital and acral areas in particular can cause significant morbidity. In cases like these, dermoscopy helps the physician, and enables avoidance of unnecessary excisions in benign tumors36,37,38. Furthermore, dermoscopy makes follow-up of lesions which have a high risk of converting to malignant melanoma, like melanocytic nevus, by physicians safer.
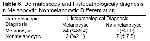
Besides being an easy-to-use, non-invasive and inexpensive diagnostic method in the diagnosis of pigmented skin lesions, dermoscopy also increases the diagnostic accuracy of clinical examination2-4,17,39-43. In a study including 107 cases with clinically suspected melanocytic skin lesions, Ferrara et al.17 reported that dermatoscopic images and histopathology of lesions were consistent. Burroni et al.39 in their study of 174 cases with pigmented skin lesions established that 71.8% of dermatoscopic pre-diagnoses were consistent with their respective histopathologies. Piccolo et al.40 reported the sensitivity and specificity of digital dermoscopy in the diagnosis of pigmented skin lesions to be 92% and 99%, respectively, for an experienced physician. However, in their study including 9004 pigmented skin lesions, Kittler et al.41 reported that dermoscopy increased the diagnostic accuracy of clinical examination by 35% and that dermoscopy was 89% sensitive and 79% specific in diagnosis. In our study when histopathologic diagnoses of 94 pigmented skin lesions were compared, we found that 63 were consistent with the clinical examination and 82 were consistent with dermoscopy.
In conclusion, dermoscopy is an easy method that is used in the diagnosis and benign-malignant differentiation of pigmented skin lesions. Dermoscopy not only is agreeable for the patients in terms of early diagnosis, excision and prognosis of malignant lesions, but also offers both the physician and the patients a chance of easy follow-up by preventing unnecessary surgical interventions to low-risk melanocytic lesions.