The present study was designed to isolate and identify the causative agent(s) of clinical mastitis cases encountered in the study region and to determine the therapeutic effect of ozone gas treatment, employed as an alternative to antibiotic therapy, in these cases.
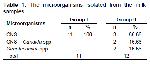
CNS are minor mastitis agents, which are frequently isolated all over the world. They are natural saprophytes found in the skin of the teats, and under favourable conditions they colonize the teat canal. In general, CNS are known to cause subclinical mastitis, but they may also cause clinical mastitis. Varying symptoms are observed in CNS-induced mastitis cases, yet the inflammation observed in these cases is of moderate severity. Random sampling in Finland revealed an isolation rate of 50% for CNS. Again, in Finland, CNS were isolated at the highest rate (18%) from clinical mastitis cases, in particular from cases of moderate severity 13,14. The isolation rate of CNS from clinical mastitis cases has been reported as 17% in Switzerland 15 and 9% in Israel 16. In the present study, the microbiological inoculation of the 23 milk samples, resulted in the isolation of CNS from 19 (82.60%) of the samples and both CNS and Candida spp. from 2 (8.69%) of the samples. The isolation rate of both CNS and Candida spp. being much higher than the rates previously reported by other researchers was noteworthy.
In cases of acute clinical mastitis, treatment should firstly focus on signs such as depression, progressive dehydration, fatigue and increased body temperature 17. Treated animals should be given an adequate volume of isotonic electrolyte solutions by IV route within a period of 1-2 hours. Fluid therapy restores the vital fluids of the animals and dilutes the toxins. In order to neutralize the effects of the prostaglandins generated as a result of inflammation, it is required to administer nonsteroidal anti-inflammatory drugs 4,18. Furthermore, in order to ensure a better distribution of the drugs administered by intramammary route, it is suggested that proteolytic enzyme preparations be administered to lyse the epithelial sloughing, blood clots, flakes and pus, and thereby, to help clear the blocked ducts 18,19. In the present study, after the inflamed quarters were milked and emptied, a proteolytic enzyme preparation was administered into the udder to help clear the ducts that were blocked due to inflammation products, and this procedure was repeated throughout the treatment period. For treatment, firstly, the animals showing signs suggestive of a deteriorated general medical condition, such as a body temperature of ≥39ºC, depression, short and rapid respiration, tremor, fatigue and anorexia, were administered 5-10 L of isotonic electrolyte solutions and 30% dextrose solution by IV route within 1-2 h, as well as an antihistaminic and nonsteroidal anti-inflammatory drugs. Non-steroidal anti-inflammatory drugs were administered to neutralize the effects of the prostaglandins generated as a result of inflammation. No mortality was observed in any of the groups throughout the study period.
In clinical mastitis cases, in order to prevent severe tissue damage, it is required to rapidly eliminate the infectious agent from the body. Reports indicate that the most effective method of rapidly eliminating the infectious agent is to administer a combination of parenteral and intramammary antibiotics 5. It has been reported that the bacteriological cure rates of clinical mastitis cases caused by Gram-positive bacteria range from 15.4% to 91.6%, depending on the intervention time, type of antibiotic used for treatment, and administration route and administration period of the antibiotic 20.
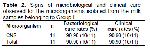
Baştan et al. 21 reported the clinical and bacteriological cure rates they achieved with the administration of a combination of intramammary amoxicillin + clavulanic acid + prednisolone and systemic amoxicillin + clavulanic acid for the treatment of acute mastitis as 84% and 88%, respectively. In the present study, the animals included in the antibiotic treatment group were administered with a parenteral antibiotic preparation containing benzylpenicillin procaine and dihydrostreptomycin sulphate and an anti-mastitis preparation containing novobiocin sodium, neomycin sulphate, procaine penicillin, dihydrostreptomycin sulphate and prednisolone into the inflamed quarters. The bacteriological and clinical cure rates achieved with this treatment regimen were both determined as 90.90%. Researchers 22,23 have reported that a bacteriological cure rate ranging between 70-90% is achieved with the use of beta-lactam antibiotics in the treatment of CNS-induced mastitis cases.
Reports indicate that the administration of ozone gas at a dose range of 10-80 ug/ml does not cause any adverse effect 6,24. In the present study, 50 mL of an ozone/oxygen gas mixture, containing ozone at a concentration of 60 μg/mL, was aspirated from an ozone generator into a plastic syringe and infused into the teat canal at 24 h intervals for a period of 3 days.
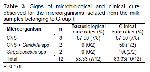
In their study on 19 cows with clinical mastitis, upon assigning the animals to two groups and infusing ozone gas aspirated from an ozone generator into the inflamed quarters of 15 of the cows and administering systemic and local antibiotics to the remaining 4, Ogata and Nagahata 12, determined that 9 (60%) of the 15 cows, which were administered ozone gas, completely healed. They suggested that ozone gas therapy could be an alternative treatment for clinical mastitis. In another study conducted by Yanliang et al. 25 30 cows with clinical mastitis were randomly allocated to 2 equal groups, such that Group I was given combined ozone gas and antibiotic therapy and Group II was given antibiotic therapy alone. In result, the researchers determined that in Groups I and II, 93.3% (14/15) and 73.33% (11/15) of the animals were cured, respectively. In the present study, the 11 cows included in Group I were administered with intramammary and systemic antibiotics, and their bacteriological and clinical cure rates were both determined as 90.90%. The 11 animals included in Group II, which were administered with ozone gas, displayed bacteriological and clinical cure rates of 58.33% and 83.33%, respectively. The cure rates achieved in the group, which was administered with ozone gas in the present study, were found to be higher than the cure rate reported by Ogata and Nagahata 12 and lower than the cure rate reported by Yanliang et al. 25 for animals administered with combined antibiotic and ozone gas therapy.
In a research conducted on 79 infected udder lobes belonging to 32 lactating cows with clinical mastitis, Enginler et al. 26 randomly assigned the animals to 5 groups and administered Group I with 100 mL of an ozone/oxygen gas mixture, containing ozone at a concentration of 70 μg/mL, into the teat canal at 24 h intervals for a period of 7 days, Group II with cephalosporin by intramuscular route for a period of 5 days, Group III with an ozone/oxygen gas mixture containing ozone at a concentration of 70 μg/mL + antibiotics, Group IV with an ozone/oxygen gas mixture containing ozone at a concentration of 30 μg/mL, and Group V with an ozone/oxygen gas mixture containing ozone at a concentration of 60 μg/mL. The general medical condition of the animals was determined to normalize in Groups I, III and V, and the best clinical and microbiological cure results were achieved in the group, which was administered with a combination of an antibiotic and a high concentration of ozone gas. In the present study, the infected quarters were infused with 50 ml of an ozone/oxygen gas mixture, containing ozone at a concentration of 60 μg/mL, at 24 h intervals for a period of 3 days. The general medical condition of all of the animals returned to normal and the bacteriological and clinical cure rates were determined as 58.33% and 83.33%, respectively. In the present study, the treatment period was shorter than that of the study conducted by Enginler et al. 26 and the amount of ozone gas used for treatment was less than that given to Groups I and V and equal to that administered to Group IV by Enginler et al. 26. The results obtained in the present study being better than the results achieved by Enginler et al. 26 in Group IV with the administration of an equal amount of ozone gas for a longer time period demonstrated the significance of the restoration of the general medical condition in the first place in animals with acute clinical mastitis.
Streptococci are ubiquitous bacteria and major mastitis agents. The most significant species of this genus are S. agalactia, S .dysgalactia, and S. uberis 27. In their study in cows with acute clinical mastitis, Ogata and Nagahata 12 determined that S. uberis was the microorganism resistant to ozone gas administered by intramammary route. In the present study, Streptococcus spp. were isolated from 2 milk samples belonging to the group administered with ozone gas and no subspecies was able to be identified. Treatment with ozone gas yielded bacteriological and clinical cure rates of 0% and 100%, respectively. Thus, it was determined that ozone gas did not have any therapeutic effect in mastitis cases caused by Streptococcus spp.
Candida spp. are classified as environmental mastitis agents. They emerge after the long-term use of antibiotics, and it is reported that antibiotics create a favourable environment for the growth of Candida spp.. Furthermore, they are transmitted with contaminated cannulae 28. In the present study, Candida spp. grew in 2 milk samples belonging to the group administered with ozone gas, and post-treatment isolation showed that Candida spp. grew once more in these two samples after ozone therapy.
As a result, it was concluded that the intramammary administration of ozone gas was very effective in the treatment of CNS-induced acute clinical mastitis cases by enabling both bacteriological and clinical cure, and that ozone could be used as an alternative to antibiotics. On the other hand, ozone gas was found to show no therapeutic effect in mastitis cases caused by Streptococcus spp. and Candida spp..